Mycobacterium tuberculosis (Mtb), the bacterium which causes tuberculosis (TB) in humans, is the most devastating infectious agent of mortality worldwide after HIV. It is air-borne and is carried by one third of all humans and kills nearly two million people annually. Synergy with the human immunodeficiency virus (HIV), along with the emergence of multidrug resistant strains (MDR-TB) , has reaffirmed Mtb as a primary public health threat (Time Magazine Oct. 2008).
MDR-TB (Multidrug-resistant) strains are resistant to at least two drugs: isoniazid and rifampicin. The World Health Organization (WHO) reported that a third of the 440,000 people who were infected with a multi-drug resistant strain in 2008, died (The Guardian Weekly, March 26-Apr. 1, 2010). An international study on 1,278 patients (Peru, the Philippines, South Korea, Russia, Estonia, Latvia, South Africa and Thailand) published in the Lancet in 2012 revealed that bacteria from infected people resistant to the current classical treatments are widely found. A staggering 43.7% of the 1,278 patients did not respond to at least one so-called second-line drug, used when the most popular medicines fail with results varying from 33.3% in Thailand to 62% in Latvia (The Economist, Aug. 31, 2012).
Existing treatments are relatively ineffective, have significant side effects and must be taken for a of long period of time. They are expensive and often in short supply as these drugs do not constitute an attractive market for businesses. This is even more of a problem for drugs known to cure MDR forms of TB (Financial Times, March 24, 2011). However, on July 23, 2012, The Lancet published encouraging new data about a drug combination called PaMZ whcih eliminated more than 99 percent of the bacteria within two weeks in a 85-person study. The research was executed at Stellenbosch University in Cape Town and funded by The Global Alliance for TB Drug Development, a New York-based non-profit organization supported by the Bill and Melinda Gates Foundation. Since PaMZ doesn’t contain isoniazid or rifampicin, the two main medicines used against TB, researchers hope that it may also provide a much-needed weapon against the MDR-TB strains (Business Week, 23 July 2012 ).
Extensively drug resistant strains (XDR-TB) are even more of a concern since they are not only resistant to the same drugs as the MDR-TB strains but are also resistant to any fluoroquinolone drug, and at least one of the following second-line drugs: amikacin, kanamycin or capreomycin. These strains were noticed worldwide in 2006 after the death of 52 out of 53 patients in KwaZulu-Natal, South Africa. Fifty-eight countries had confirmed at least one case of XDR-TB in 2010 (The Guardian Weekly, March 26-Apr. 1, 2010). In the 2012 international study mentioned above, an average of 6.7% of patients carried XDR-TB The numbers ranged from 0.8% in the Philippines to 15.2% in South Korea. Researchers noted that the occurence of XDR-TB was higher in countries where the second-line drugs had been in use the longest. These observations suggest that XDR-TB is likely to increase in regions where these drugs have only recently been used (The Economist, Aug. 31, 2012).
An XDR-TB strains leave TB patients virtually untreatable with current medicines unless they can afford special treatments that cost around $100,000. XDR-TB strains have now been isolated throughout the world (see map above) (XDRTB.org). While these MDR and XDR-TB strains amount to approximately 5% of the total annual cases of TB registered in the world, they represent an unprecedented threat to our health systems.
A rare strain of extremely drug-resistant, XXDR-TB (only a handful of other people in the world are thought to have had it), is even more aggressive and difficult to treat than XDR-TB. Associated Press recently learned about the case of a young patient infected with an XXDR-TB strain who had to be treated during 19 months at a Florida hospital using experimental protocols at the cost of $500,000 (Time Magazine, Dec. 2009). In January 2012, reports of a deadly form of tuberculosis completely resistant to all drugs normally used to cure it, was reported in India and called totally drug-resistant tuberculosis (TDR-TB). Previous cases had been identified in Italy in 2007 and in Iran in 2009 (The Scientist, Jan. 16, 2012).
The World Health Organization (WHO) has declared TB a global health emergency: “novel therapeutics are urgently required to target persistent bacilli and to contribute to more effective treatments of TB” (WHO) .The WHO held its first drug-resistant TB conference in Beijing in April 2009. Although more than half of the cases of drug-resistant TB are in China and India, the highest concentrations of 2008 cases were recorded in Murmansk, Russia while the highest concentration of 2007 cases were in Azerbaijan (The Guardian Weekly, March 26-Apr. 1, 2010). The WHO is warning that there is a real risk that resistant strains of TB spread worldwide.
The Centre for TB Research (CTBR) located at the University of British Columbia in Vancouver, regroups scientists from various disciplines who study Mycobacterium tuberculosis to understand how it infects and establishes itself in humans. Such knowledge is key to the development of effective new drugs against the bacterium.
In Canada, First Nations and Inuit communities are at an especially high risk due to poor living conditions and nutrition, overcrowded housing and limited access to health care (Health Canada). A 2010 report from the Public Health Agency of Canada showed that TB infection rates in native populations are 31 times that of non-aboriginal Canadians (Globe and Mail, Mar. 2010). In Nunavut alone, the infection rate is 62 times the Canadian average. “We are a rich, developed nation that has the resources to solve the problem in Nunavut if we choose to employ them,” said Dr. Matthew Stanbrook, a respirologist at Toronto Western Hospital. “The fact that we have failed to do so, not just once but over a century, should be an embarrassment to every Canadian.“ (CBC News, Feb. 14, 2011). However, some statistics can be even worse: in 2009 cases of tuberculosis reached a 30-year high in Manitoba where some northern native communities were shown to have 600 cases of TB per 100,000 population while Canada’s national average is of 5 cases of TB per 100,000 population. By contrast Bangladesh’s national average is 400 cases per 100,000 (National Post, March 2010). Provincial and federal governments need to support initiatives aimed at improving housing conditions and eliminating poverty according to Grand Chief Ron Evans from the Assembly of Manitoba Chiefs (National Post, March 2010).
In Canada’s largest city, Toronto, the death rate from tuberculosis in homeless people is also alarming. A 10-year study looking into the homeless in Toronto found that one in five homeless people with tuberculosis died within a year of their diagnosis, a rate which is three to four times higher than what is generally seen in the general population according to Dr. Kamran Khan, an infectious disease physician and scientist at St. Michael’s Hospital. Khan says Toronto’s homeless shelters have been lucky because a drug resistant strain of TB has not entered the shelter system. But, Khan warned if a multi-drug resistant TB strain did, it could set off an outbreak that would become very difficult to control.
These are all warning signs that our current handle on the treatment of TB in vulnerable populations needs to be improved.
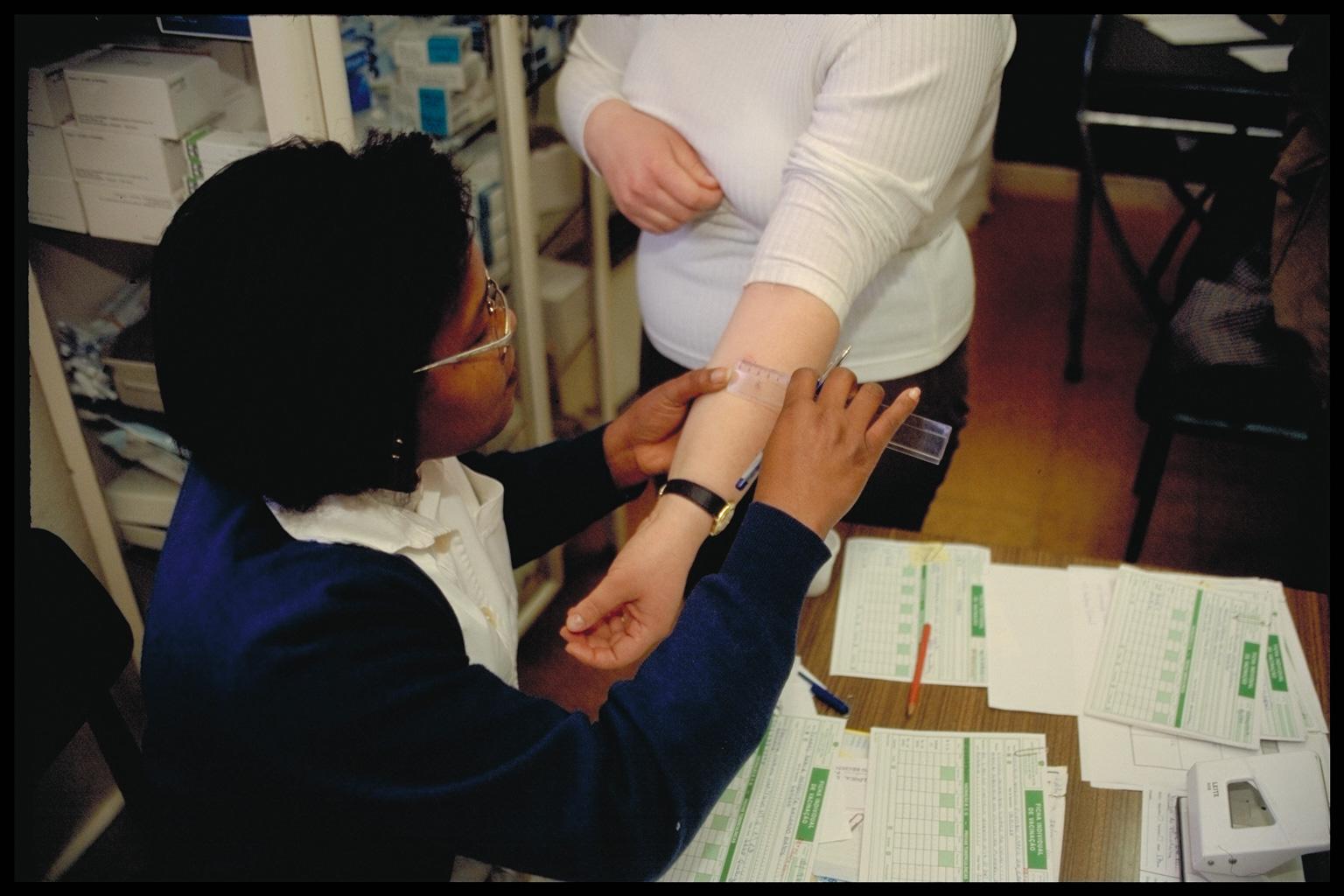

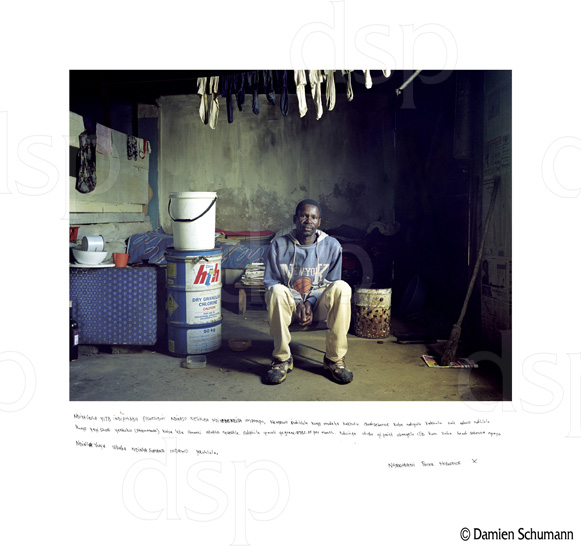 Pictures compliments of Lung Health Image Library
Pictures compliments of Lung Health Image Library